The Forgotten Truth of Trauma in Psychology
From Janet to Freud: A Lost Lineage of Trauma Understanding
Before Freud became the icon of psychoanalysis, he was a student of the French neurologist and psychologist Pierre Janet, widely credited as one of the earliest theorists of dissociation. Janet’s work with hysterical patients revealed that traumatic events, especially those occurring in early life, could fragment consciousness and lead to the development of discrete self-states—a phenomenon we now recognize as dissociative identity disorder (DID) and related conditions.
Freud, influenced by Janet and initially deeply curious about trauma, began collecting case studies of his own. He noted the remarkable regularity with which his clients—especially women—reported early sexual violations, often perpetrated by fathers, brothers, or other male authority figures. These disclosures formed the foundation of what became known as Freud’s “seduction theory.”
In letters and early papers, Freud seemed to acknowledge the devastating impact of abuse, writing in 1896:
"I therefore put forward the thesis that at the bottom of every case of hysteria there are one or more occurrences of premature sexual experience..."
He was inching toward the radical conclusion that trauma, particularly sexual trauma, was the root of many psychological symptoms. The implications were massive—not just scientifically, but socially.
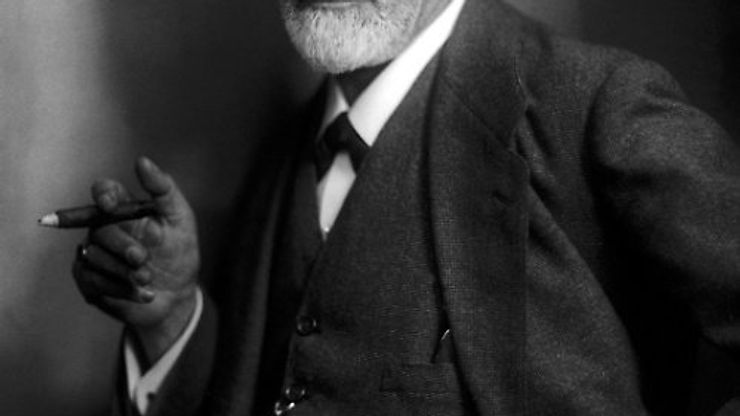
The Collapse of Courage: Freud’s Retreat from Truth
Faced with mounting pressure from his colleagues in Viennese medical and academic society, Freud made a dramatic pivot. In 1897, he wrote to his confidant Wilhelm Fliess:
“I no longer believe in my neurotica.”
This moment marks one of the most tragic betrayals in the history of mental health. Freud rejected the idea that his clients had actually been abused and instead posited that these memories were unconscious wishes or fantasies—an internal drama, rather than external fact. The implications were profound:
- Trauma was reframed as fiction.
- Survivors became hysterics, liars, or neurotics.
- The real societal structures that perpetuated abuse were left intact.
This abandonment was not rooted in evidence but in career preservation. As Jeffrey Masson, author of The Assault on Truth, notes: “Freud knew that if he held firm to the seduction theory, he would have been cast out of the medical community.” The cost of telling the truth was too high.
From Dissociation to “Split Minds”: The Invention of Schizophrenia
The term “schizophrenia” was coined in 1911 by Swiss psychiatrist Eugen Bleuler, derived from Greek roots meaning “split” (schizo) and “mind” (phren). Contrary to modern usage, it was not originally meant to describe hallucinations or delusions, but rather a disconnection in thought, affect, and identity—symptoms that overlap significantly with dissociative disorders.
Author and psychiatrist Colin Ross has written extensively on how the rise of schizophrenia as a diagnosis eclipsed dissociation and trauma in the 20th century. In his book The Osiris Complex, Ross argues that many individuals historically diagnosed with schizophrenia would more accurately meet criteria for DID or other trauma-based conditions today. He calls this the “false schizophrenia epidemic.”
By labeling these presentations as biologically driven psychosis, psychiatry effectively medicalized dissociation and further distanced itself from the trauma narrative. The split mind, once understood as a reaction to unbearable reality, became a genetic defect or chemical imbalance.

Reclaiming the Narrative Through EMDR and KAP
In more recent decades, therapies like Eye Movement Desensitization and Reprocessing (EMDR) and Ketamine-Assisted Psychotherapy (KAP) have begun to restore what Freud and others buried. These modalities recognize what survivors have always known:
- Trauma fragments the self.
- Healing requires integration.
- Dissociation is not madness—it is protection.
Uri Bergmann, in his book Neurobiological Foundations for EMDR Practice, situates EMDR within a trauma-informed and dissociation-aware framework. He explains how EMDR helps reintegrate traumatic memories into narrative memory, bridging the gap between implicit somatic memory and explicit understanding. EMDR has been shown to activate bilateral brain processing, restoring coherence to what was previously fragmented.
KAP takes this even further. Ketamine, originally developed as an anesthetic, produces a temporary deactivation of the brain’s Default Mode Network (DMN)—the area responsible for ego, rumination, and self-referential thought. With the DMN offline, clients often experience a lifting of the veil: profound emotional clarity, spiritual connection, and access to exiled parts of the self. Dissociation, in this context, becomes a portal rather than a pathology.
KAP supports healing through multiple mechanisms:
- Biochemically, it boosts glutamate and promotes neuroplasticity.
- Psychologically, it softens defenses and allows for deep emotional access.
- Archetypally, it opens the door to symbolic healing, often echoing the soul retrieval processes found in shamanic traditions.
Breaking the Legacy of Silence
When Freud chose to reject the reality of abuse, he didn’t just betray his patients—he set a precedent for decades of psychiatric denial. But today, clinicians are circling back. We are re-validating the stories that were once dismissed and building frameworks that honor the complexity of trauma.
Whether through EMDR, KAP, parts work, or somatic therapies, we are learning to listen again. To the body. To the symptoms. To the voices within. And perhaps, most importantly—to the survivors who never stopped telling the truth.
Sources & Further Reading:
- Masson, J. (1984). The Assault on Truth: Freud’s Suppression of the Seduction Theory.
- Ross, C. (1994). The Osiris Complex: Case Studies in Multiple Personality Disorder.
- Bergmann, U. (2012). Neurobiological Foundations for EMDR Practice.
- Ellenberger, H. (1970). The Discovery of the Unconscious: The History and Evolution of Dynamic Psychiatry.